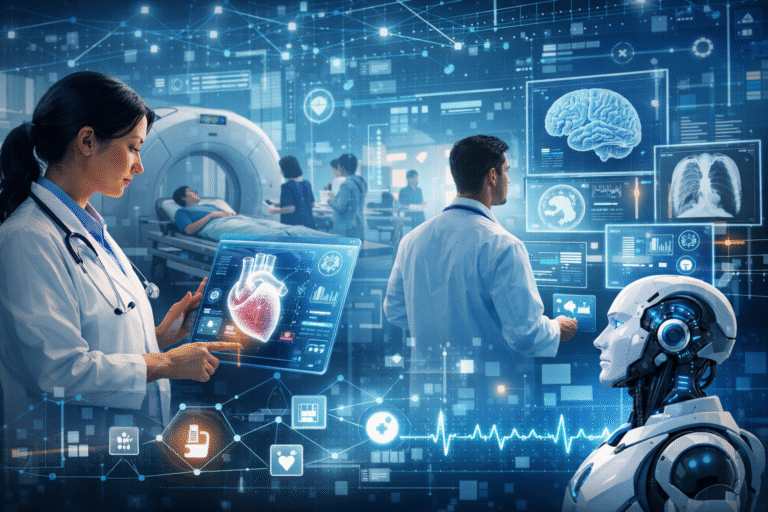
Telemedicine is no longer a research-based extension of the healthcare system. Telemedicine has become a standard means of delivery—used by healthcare providers to enhance access, continuity of care, and efficiency. But developing a telemedicine app in 2026 is more than just incorporating video communication and appointment scheduling.
It requires a focus on integrating technology with real-world clinical processes, regulatory requirements, and long-term viability.
This guide provides a step-by-step guide on how to develop a telemedicine app based on a practical approach.
What Is Telemedicine App Development?
Telemedicine app development is the process of designing and developing digital solutions for remote clinical consultations between patients and healthcare professionals. Telemedicine apps are used for consultations, follow-ups, monitoring, documentation, and payment while ensuring clinical safety and integrity.
Telemedicine apps are different from other types of apps because they are used in a regulated space and need to integrate with the existing healthcare infrastructure.
Why Telemedicine Is Emerging as Essential Healthcare Infrastructure
Telemedicine is no longer a nicety but a necessity. It has become a crucial element in the strategy that healthcare infrastructure adopts to deal with access, capacity, and continuity.
Telemedicine apps are being increasingly employed for:
- Minimizing unnecessary in-person visits
- Enhancing adherence to follow-ups
- Optimizing use of clinician time
- Extending healthcare beyond physical infrastructure
In the year 2026, successful telemedicine platforms will be those that enable hybrid care strategies, data-informed decision support, and sustainable operational performance as opposed to isolated telemedicine encounters.
Why Telemedicine Is Emerging as Essential Healthcare Infrastructure
Telemedicine is no longer a nicety but a necessity. It has become a crucial element in the strategy that healthcare infrastructure adopts to deal with access, capacity, and continuity.
Telemedicine apps are being increasingly employed for:
- Minimizing unnecessary in-person visits
- Enhancing adherence to follow-ups
- Optimizing use of clinician time
- Extending healthcare beyond physical infrastructure
In the year 2026, successful telemedicine platforms will be those that enable hybrid care strategies, data-informed decision support, and sustainable operational performance as opposed to isolated telemedicine encounters.
A Practical Framework for Telemedicine App Development
Step 1: Define the Exact Clinical Use Case
Each successful telemedicine solution begins with a specific clinical problem in mind. Vague objectives such as “telemedicine” are not specific enough for sound product design decisions.
Key questions to answer:
Who is the target user—patient, provider, or care coordinator?
What clinical outcome is to be improved?
Which interactions are truly better off remote?
Step 2: Choose the Right Telemedicine Care Model
Telemedicine solutions are based on one or more of the following models:
- Real-time consultation through video or audio communication
- Asynchronous communication through structured messaging
- Remote patient monitoring through connected devices
Although there are hybrid solutions, the first priority should be on the primary use case and not attempt to address all models simultaneously.
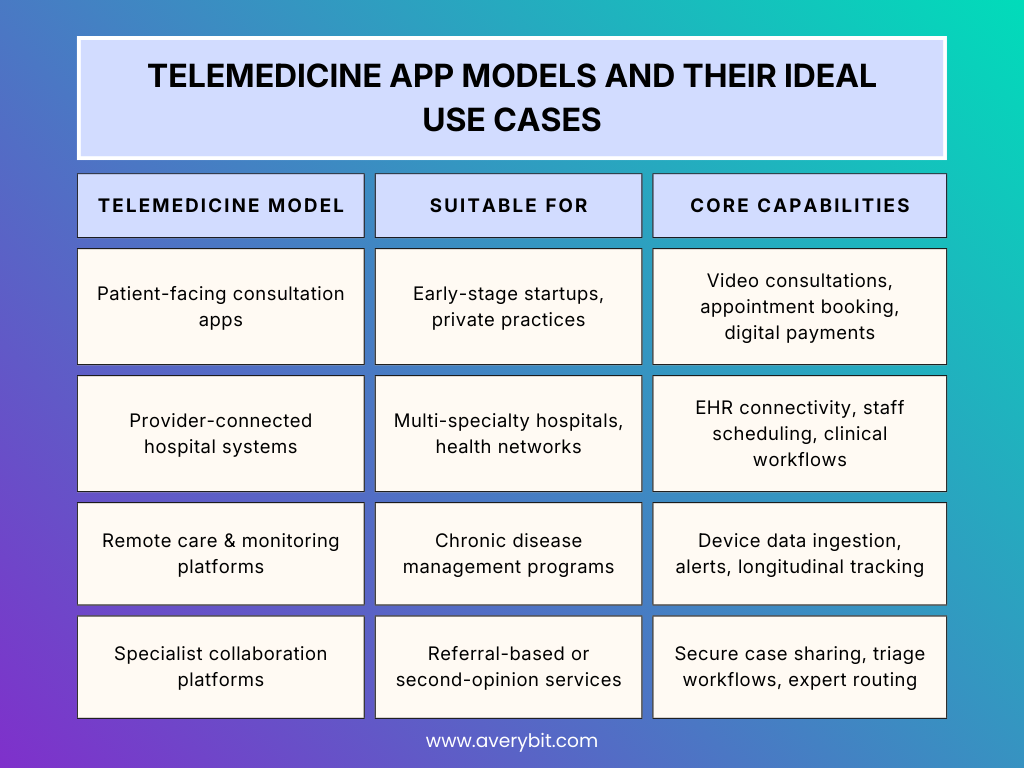
Not every telemedicine app solves the same problem. Choosing the wrong model early often leads to expensive rebuilds later.
Step 3: Aligning Features with the Real World
Features should align with the real world of how healthcare professionals already operate, rather than trying to change their behavior.
Primary functionality will include:
- Secure video conferencing with fallbacks
- Appointment scheduling and queuing system
- Structured clinical documentation system
- Secure patient messaging system
- Integrated billing or payment system
The goal is to reduce administrative friction, not introduce parallel systems.
Custom-Built Telemedicine Software vs Ready-Made Platforms
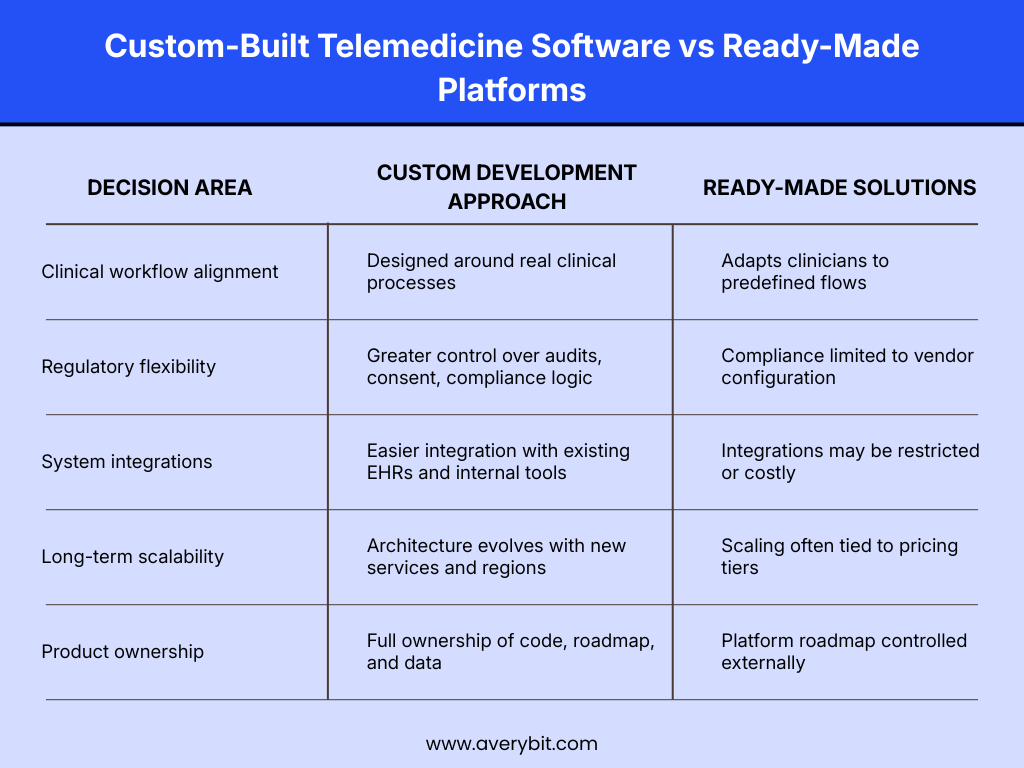
Off-the-shelf tools can be useful for pilots, but organisations planning long-term digital care delivery usually outgrow them faster than expected.
Step 4: Integrating Privacy, Security, and Consent into the Product
Security and compliance are architectural issues, not checklists. Telemedicine applications involve sensitive patient data and therefore require appropriate design.
Some important factors include:
- Data encryption in transit and at rest
- Role-based access control
- Consent workflows
- Audit trails for clinical and administrative activities
These factors are addressed early on to prevent delays and loss of trust down the line.
Step 5: Integrating Telemedicine with Existing Healthcare Systems
A telemedicine application needs to work with existing healthcare systems for continuity of care.
Some common integration requirements include:
- Synchronizing patient demographic and clinical data
- Storing consultation notes back into the system of record
- Accessing patient medication lists or lab results
Interoperability reduces duplication and improves clinical accuracy.
Step 6: UX Design for Patients and Healthcare Professionals
Telemedicine apps are used by multiple audiences with varying needs. Patients want simplicity and reassurance, whereas healthcare professionals want speed and simplicity.
Good UX design involves:
- Few steps to start or join a consultation
- Clear display of medical data
- Accessibility on multiple devices
- Error prevention in critical tasks
Good UX design enhances adoption and support efficiency.
Step 7: Choosing Between an MVP and a Full Telemedicine Solution
Too many features at once can cause project delays and make the solution more complicated. A well-structured MVP allows for rapid validation of project assumptions.
An MVP will have:
- One primary consultation experience
- Basic compliance and security features
- Restricted but stable integration points
Growth should be informed by actual user data, not assumptions.
Step 8: Testing, Clinical Validation, and Quality Assurance
Testing a telemedicine app is more than just making sure the app is functional.
It must take into consideration clinical safety, system reliability, and practical usage.
Testing for the telemedicine app involves:
- Video and communication system stability
- Data accuracy for all integrations
- Permission and access logic
- Failure modes, such as network dropout
Clinical validation of the telemedicine app ensures it facilitates safe care delivery.
Step 9: Deployment Strategy, Billing, and Long-Term Value
Product deployment begins the product life cycle, not the end of it. Optimizing the product is the key.
After the deployment, the following are some of the most important priorities:
- Performance and availability management
- Billing and reimbursement management
- Usage analytics
- Continuous improvement
A post-launch strategy will help transform the telemedicine app into a healthcare asset.
Custom Development vs. Telemedicine Platforms
Telemedicine platforms can speed up initial deployment but might hinder flexibility in the long run. Custom telemedicine app development provides more flexibility in terms of workflow, integration, and scalability.
The answer to the question of what to do depends on:
- The complexity of the clinical problem
- The level of integration required
- The long-term product strategy
Organizations seeking to differentiate themselves might find custom development more valuable.
Challenges and How to Overcome Them
Some common challenges include:
- Adding too many features to the telemedicine platform
- Underestimating the complexity of integration
- Taking compliance for granted
- Not considering clinician input during the design phase
- Early planning and collaboration can help overcome these challenges.
Conclusion: Developing a Sustainable Telemedicine Platform
Developing a telemedicine app in 2026 requires more than just technical know-how. It requires strategic thinking, workflow understanding, and a long-term perspective.
Successful telemedicine platforms are those that are developed around real clinical needs, a strong security foundation, and scalable architecture, rather than trends and assumptions.
If you are considering the next steps for your telemedicine product, a thoughtful approach and skilled execution can make all the difference between adoption and obscurity.
Common Challenges and How to Avoid Them
Common challenges include:
Overloading the platform with unnecessary features